دوست داری رژیم بگیری ؟

Part 1: Assessment of Vitamins and Minerals
Part1: Assessment of Vitamins
1-Definition of Vitamins
• Vitamins are natural organic substances in food.
• Small amounts of them are required for the physiological needs of the body.
• They are not synthesized in sufficient quantities in the human body.
• Lack of vitamins or vitamin deficiency can lead to some symptoms, which are reversible through adequate intake and storing of sufficient quantities.
2-The Purposes of Vitamin Assessment
• Defining the role of nutrition and clinical tests in assessing the nutritional status of vitamins
• Accurate interpretation of the laboratory tests conducted for assessing the nutritional status of vitamins.
• Summarizing the analytic methods used in assessing the nutritional status of vitamins.
3-The Necessity of Assessing Vitamins
As mentioned, vitamins are organic substances that are not synthesized in the body and their deficiency or toxicity can cause different illnesses in humans. In contrast, sufficient amounts of vitamins in the body can prevent illnesses and clinical symptoms, as well as, promoting health, efficient growth and optimal functioning of organs. Deficiency or toxicity of different vitamins with clinical symptoms and the diseases caused by them are talked about here:
Vitamin A
Vitamin A Deficiency
Vitamin A deficiency is caused as a result of inadequate intake of vitamin A or its precursors (carotenoids). Secondary deficiency is caused as a result of inadequate intake of fats, liver or pancreas failure, liver disease, protein-energy malnutrition or zinc deficiency.
Vitamin A deficiency is the most common cause of blindness in developing countries and about 250 million children are at risk of it. 250000 to 500000 cases of blindness occur as a result of vitamin A deficiency each year. One of the vitamin A deficiency symptoms is impaired vision as a result of reduced visual pigments. The clinical manifestation of this condition is night blindness or nyctalopia. The inability of dark adaptation (adaptation while moving from a bright place to a dark place, such as driving at night or going from a light room to a dark room) is a result of retinal dysfunction. Individuals with nyctalopia have weak visual differentiation and may not be able to see in half-dark or dim places. In addition to measuring vitamin A plasma levels, dark adaptation test is one of the recommended methods for evaluating vitamin A efficiency.
Prolonged vitamin A deficiency results in dysfunction of several organs; such as, birth defects, impairment in spermatogenesis, miscarriage, anemia, immune disorders and increased risk of bone fracture. It can also cause keratinization of the mucus membranes of the respiratory, gastrointestinal and urinary tracts, and also, skin and eye epithelium. Clinical presentations are weak growth, blindness caused by xerophthalmia, corneal lesion and nasal obstruction (caused by excessive growth of skull).
Vitamin A deficiency causes changes in skin including follicular hyperkeratosis. Blockage of hair follicles with Keratin will cause the appearance of toad or goose skin. In this condition the skin is dry, flaky and rough. It is first only found on upper arms and thighs but in advanced stages it can affect the entire body.
Lack of integrity of mucous membranes as a result of vitamin A deficiency increases the risk of bacterial, viral or parasitic infections. Vitamin A deficiency can also cause cell-mediated immunity disorders and ultimately increase the risk of infection especially in the respiratory system.
Acute deficiency of this vitamin is treated with oral prescription of high quantities of this vitamin.
Vitamin A Toxicity
Continuous high intake of vitamin A will overwhelm the liver storage capacity and cause toxicity and eventually liver disease. Vitamin A Toxicity is characterized by changes in skin and mucus membranes. Its symptoms include dryness, redness, scaling, peeling, hair loss and brittle nails. Symptoms such as headache, nausea and vomiting have also been reported.
Thiamine (B1)
Thiamine (B1) Deficiency
Thiamine Deficiency is characterized by lack of appetite, weight loss, and cardiovascular and neurological symptoms. Thiamine Deficiency eventually leads to Beriberi; its symptoms include mental confusion, muscle atrophy, peripheral neuropathy, bradycardia, cardiomegaly and edema. Also, the dry type is usually accompanied by lack of energy and low activity.
Beriberi is more common in poor regions; where people have a diet high in white rice or who eat raw fish. In addition, thiamine is necessary for the metabolism and detoxification of alcohol; therefore, alcohol consumers need more thiamine. Some elderly people are at risk of thiamine deficiency, because of poor diet and long-term consumption of diuretics, due to hypertension or heart failure.
People with thiamine deficiency develop a type of encephalopathy called the Wernicke-Korsakoff syndrome; its symptoms vary from confusion to coma. Assessing thiamine status can be done by determining the activity of transketolase enzyme in red-blood cells and measuring serum or urine levels of thiamine.
Thiamine (B1) Toxicity
High intake (1000 times more than the nutritional needs) of thiamine hydrochloride, the commercial form of thiamine, will cause death through stopping the respiration center. Administration of 100 times more than the needed amount via injection, can cause headache, seizure, muscle weakness, arrhythmia and allergic reactions.
Riboflavin (Vitamin B2)
Riboflavin (B2) Deficiency
Riboflavin deficiency will appear after months of insufficient intake. Its primary symptoms include photophobia, burning and itching of the eys, tearing, loss of clear sight, lip fissures, inflammation and red patches in the corners of the mouth (angular stomatitis or angular cheilitis), oily scaly skin rashes on the nasolabial fold, scrotum and vulva, inflamed red tongue and peripheral neuropathy. Riboflavin deficiency usually occurs in people with malnutrition, in combination with deficiency of other water-soluble vitamins such as thiamine and niacin.
Riboflavin toxicity
Riboflavin is not known as a toxic agent. Oral consumption of high quantities is considered non-toxic but is not recommended.
Niacin (Vitamin B3)
Niacin (B3) Deficiency
Primary symptoms of niacin deficiency include muscle weakness, low appetite, indigestion and rash. Severe niacin deficiency leads to pellagra, which is characterized by dermatitis, dementia, diarrhea, tremor and painful tongue. Dermal changes are the most evident changes. Stretch marks, hyper pigmentation and scaly dermatitis are seen on the sun exposure site of the skin. Central nervous system symptoms include confusion, disorientation to time and space and neural inflammation. Gastrointestinal disorders include irritability and inflammation of the mucus membranes of mouth and the gastrointestinal tract.
The most reliable method of assessing niacin level is measuring the urinary excretion of its methylated metabolites.
Niacin (B3) Toxicity
Generally niacin toxicity is rare. However 1 to 2 grams of nicotinic acid 3 times a day (the quantities administered for lowering cholesterol levels) have side effects. The most important side effect is releasing histamine which causes flushing and can be dangerous for people with asthma and sore (however nicotine amid doesn't have these side effects).
High quantities of niacin can also be toxic for liver. Consumption of high quantities needs to be consumed with precaution, because high quantities of niacin function as a drug, not a supplement.
Pantothenic acid (Vitamin B5)
Pantothenic acid deficiency (Vitamin B5)
Pantothenic acid deficiency leads to disruption in lipid synthesis and energy production. Due to high distribution of this vitamin in foods, its deficiency is rare. However its deficiency is seen in people with severe malnutrition. Its symptoms include numbness of hand and feet, feeling of burning and numbness in feet, depression, fatigue, insomnia and weakness.
Pantothenic acid (B5) Toxicity
Pantothenic acid toxicity is negligible. No negative effect in any species has been reported as a result of consumption of high quantities of this vitamin. Very high quantities (10 grams per day) can only cause mild intestinal discomfort and diarrhea.
Pyridoxine (Vitamin B6)
Pyridoxine (B6) Deficiency
Insufficient intake of pyridoxine leads to metabolic disorders and these disorders clinically manifest as dermal and neural changes. Insufficient levels of this vitamin in brain can lead to neural disorders especially epilepsy.
Due to the existence of this vitamin in most of the foods, cases of vitamin B6 deficiency are rare. Although, it can occur during consumption of certain drugs (like Isoniazid for tuberculosis), because they cause disruption in the metabolism of pyridoxine.
Pyridoxine (B6) Toxicity
Dietary toxicity of vitamin B6 is relatively low. However, high quantities cause sensory neuropathy which is characterized by a change in walking and peripheral sensation. Many of the symptoms of vitamin B6 toxicity are like its deficiency symptoms.
Folate (Vitamin B9)
Folate (B9) deficiency
Folate deficiency causes disruption in biosynthesis of DNA and RNA, and therefore decreases cell division. It is more prominent in cells with high proliferation rate, like leucocytes, red blood cells (which causes anemia) and epithelial cells of stomach, intestine, vagina and cervix. Low levels of folate can also cause neural tube defects and psychological disorders in old age.
Folate (B9) Toxicity
No adverse effects have been recorded as a result of high oral intake of folate, but quantities over 1000 times more than the needed amount can cause epilepsy-like seizures. High levels of folate reduce the bioavailability of zinc through the formation of non-absorbable complexes in intestine. High doses of folate supplement can hide vitamin B12 deficiency.
Vitamin B12
Vitamin B12 deficiency
Vitamin B12 deficiency can cause disruption in cell proliferation through stopping DNA synthesis especially in cells with high proliferation rate, like bone marrow and intestine mucus membrane. It can also cause neurological disorders that manifest later than anemia. These disorders include progressive neuropathy with neural demyelination. Neurological disorders start from peripheral nerves and spread toward central nerves. Its symptoms include numbness, tingling, weakness in legs, psychological disorders like cognitive problems and depression. If vitamin B12 deficiency is prolonged the neural damage becomes permanent. Vitamin B12 deficiency symptoms include lemon-yellow skin color (jaundice) and beefy-red tongue (glossitis). Prolonged consumption of vegetarian diets without vitamin B12 supplementation leads to very low levels of the vitamin B12 in the circulation. Vitamin B12 deficiency and bone fractures are common among vegetarians and must be carefully monitored.
Vitamin B12 Toxicity
Vitamin B12 doesn't lead to a remarkable toxicity.
![ویتامین B]](/contents/bookables/33/Vitamin2-min.png)
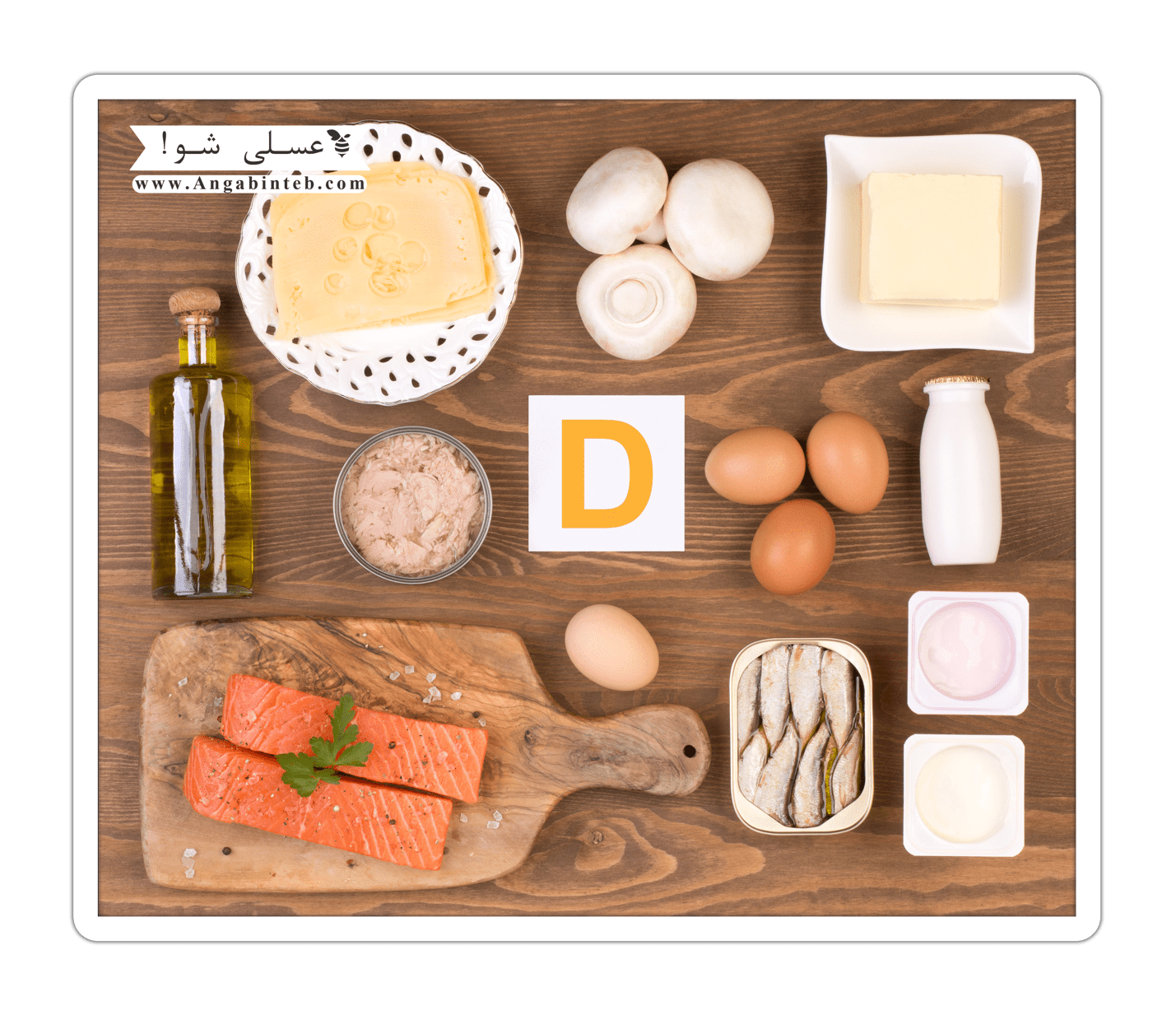
Vitamin D
Vitamin D Deficiency
Approximately 1 billion people in the world don't receive enough vitamin D levels. Black people are at higher risk of vitamin D deficiency.
Vitamin D is necessary for healthy bones; it helps the body to keep the proper level of calcium for regulation of the growth of teeth and bones. Osteoporosis, which occurs as a result of calcium and vitamin D deficiency, can lead to porous and fragile bones, which break easily. The best source of vitamin D is sunlight. Some research suggest that being exposed to sunlight 5 to 30 minutes twice a week in face, neck, arms or back can provide sufficient vitamin D levels. Sunscreen, although recommended, stops formation of vitamin D through skin. For efficient vitamin D formation by skin, spend a couple of minutes in sunlight and then apply sunscreen.
Vitamin D toxicity
Receiving extra vitamin D can cause toxicity that leads to calcification of soft tissues, like kidneys, lungs, heart and even the tympanic membrane (which can cause deafness), through increasing calcium and phosphorous levels. Patients often complain from headache and nausea. Infants who receive high quantities of vitamin D can develop gastrointestinal disorders, bone fragility and delayed growth.
Vitamin E
Vitamin E Deficiency
Clinical manifestations of vitamin E deficiency are significantly different. Neural, muscular, vascular and reproductive systems are in danger. The progress of vitamin E deficiency might take 5 to 10 years. It clinically manifests as areflexia, loss of the vibration and proprioception sense, imbalance and accommodation impairment, muscle weakness and visual disorders. Symptoms in humans are uncommon and only occur in people with malabsorption (such as, biliary obstruction and exocrine pancreatic insufficiency) and fat transportation defect.
Limited embryonic transportation of vitamin E causes low levels of vitamin E in infants’ tissues. Therefore premature infants may be at risk of vitamin E deficiency.
Vitamin E Toxicity
Vitamin E toxicity is uncommon, but in high quantities, it can reduce the body's ability for using other fat-soluble vitamins.
Vitamin K
Vitamin K Deficiency
The major symptom of vitamin K deficiency is bleeding, which in severe cases leads to life-threatening anemia. Reduction of blood prothrombin is a background factor which is characterized by increased time of blood coagulation (prothrombin time [PT]). Vitamin K deficiency is rare, but is related to fat malabsorption, destruction of intestine fleur by long-term treatment with antibiotics, and liver disease. Newborns, especially premature ones and infants who breastfed exclusively, are at risk of hypoprothrombinemia at first days of their life, due to insufficient placental transportation of vitamin K and problems in the formation of vitamin K producing microflora. Vitamin K deficiency is also related to an increased risk of distal femur fractures in old adults.
Vitamin K Toxicity
Natural forms of vitamin K show no adverse effects in any methods of administration, but the synthetic form (menadione) can be toxic in extremely high quantities, which cause jaundice and hemolytic anemia.
Vitamin C
Vitamin C Deficiency
Severe vitamin C deficiency in people who are not capable of synthesizing vitamin C leads to scurvy and in adults the symptoms appear after 45 to 80 days of deficiency. In children the vitamin C deficiency syndrome is called Möller-Barlow's syndrome. This disease is also seen in infants who are fed formula which is not saturated with vitamin C. In both cases lesions appear in mesenchymal tissues that manifest as wound recovery impairment, edema, bleeding and weakness in bones, cartilages, teeth and connective tissues.
Symptoms in adults who have scurvy include scorbutic gums (inflammation and bleeding in gums), losing teeth, sleepiness, fatigue, arthralgia in legs, muscular atrophy, dermal ulcers and different psychological changes.
Vitamin C Toxicity
Vitamin C is one of the most commonly used supplements. The adverse effects of high quantities of it are gastrointestinal disorders, diarrhea and the formation of oxalate kidney stones.


The assessment and treatment methods of vitamin and mineral deficiencies:
Treatment is depended upon the type and severity of the deficiency. Your doctor will find out the severity of the deficiency and whether there is the probability of long-term problems caused by nutritional deficiencies. They can perform further tests to check for other deficiencies before they start the treatment. The symptoms usually disappear while being on the correct diet or taking supplements.
In the case of a minor deficiency, the doctor might recommend you to change your dietary habits. For example, individuals with iron-deficiency anemia should eat more meat, egg, chicken, vegetables and beans in their diet.
If the severe deficiency exists, the doctor might refer you to a nutritionist. Nutritionists might recommend that you prepare a food reminder for a couple of weeks. When you meet with the nutritionist review your food plan and the nutritionist identify the changes that need to be done.
Usually, you will meet your nutritionist regularly. Eventually you might have to perform a test to confirm that no longer vitamin or mineral deficiencies are present.
Supplements
It is recommended that you get most of your nutrients from food but in some cases you may need to take supplements or multi-vitamins. You might also need extra supplements to help the absorption of supplements like calcium and vitamin D.
Regularity of use and the amount of the supplement used are dependent on the level of deficiency. Your doctor or nutritionist can determine this.
Before taking any dietary supplement consult your doctor.
4-Assessment of Nutritional Status of Vitamins
History: nutritional, medical, social
• Collecting information about the amount of intake and the needed amount of nutrients
• Physical examination
• Anthropometric measurements (height, weight, skinfold thickness, mid-upper arm circumference)
• Estimating protein and fat reserve
• Body composition analysis
• Biochemical tests
• Laboratory assessment of nutrients in body fluid samples
5-Vitamins' Properties
• Containing different chemical compounds.
• Different physiological functions.
• Existence in different food resources.
Vitamins might exist in a singular form:
• Vitamin C (ascorbic acid)
Though, some others have different forms:
• Vitamin A (retinol, retinal, retinaldehyde)
• Vitamin E (tocopherols, tocotrienols)
6-Vitamin's classification is based on solubility:
• Water soluble vitamins
• Fat soluble vitamins
Vitamins' solubility affect on the:
• Absorption and transportation
• Storage, toxicity and excretion
• Response to a specific disease or injury
7-Types of Vitamins
Water-soluble vitamins:
Vitamin B1 Thiamine, thiamine phosphate
Vitamin B2 Riboflavin, other Flavin's
Vitamin B3 Niacin, nicotinic acid, nicotinamide
Vitamin b6 Pyridoxine, pyridoxal, pyridoxamine
Vitamin b12 Cyanocobalamine
Vitamin C Ascorbic acid, dehydroascorbic acid
Fat-soluble vitamins:
Vitamin A Retinoid
Vitamin E Tocopherols, tocotrienols
Vitamin K phylloquinone, menaquinone
Vitamin D Cholecalciferol, ergocalcierol
8- Laboratory Assessment of Vitamins
Laboratory assessment of vitamins is a suitable method for assessment of the nutritional status (deficiency, sufficiency or toxicity of vitamins).
Using Test Results
Nutritionists search about vitamins intake to identify the needed quantities of vitamins – in food or supplements – which the individual should take for health and prevention of diseases?
Measuring Vitamin Intake:
• Dietary reference intake (DRI) – reference intake quantities or estimating the food quantity of each of the main nutrients
• Recommended dietary allowances (RDA) – the mean daily dietary quantity of the nutrients that is sufficient for the majority (97%-98%) of healthy people which are classified based on age, sex and physiological needs.
In the clinical laboratories the concentration of vitamins in body fluids is measured. Although in some cases the relationship between consumption and concentration might not be very clear.
9-Assessment of Vitamins' Status
Laboratory assessment of vitamins concentration might be helpful in clinical assessment of the patient if these two items be identified:
• The needed amount of each vitamin
• Reference intake quantities
Important items in assessment of the nutritional status of vitamins are classified as the sample related factors and patient status factors:
Sample related factors:
• Collection, processing and storing
• Type (blood, serum, plasma or urea)
• Measuring extracellular concentration of micronutrients, including vitamins, is an indirect and relatively insensitive index for the status of nutrients. Also, it is enough for determining deficiency or toxicity. And in some cases it is the reliable index of the vitamins status.
Patient status factors:
• Fasting/not fasting
• Taking vitamin supplements
• Age
• sex
• Ill/healthy
• Geography/culture, diet

Vitamins are photosensitive compounds; therefore, collection, transportation and storage of vitamins are important for integrity of the sample.
Vitamins concentration in biological fluids is reported as pico molar (pmol/L) to micro molar (mmol/L).
Analytic methods for results of the test must be precise, sensitive and specific.
10-Sample (collection, processing and transportation)
• Samples are sensitive to light and temperature. Therefore, sunlight must be avoided while collecting, storing and transporting the sample. One hour after collecting the sample, plasma should be separated from the cells. Also, the appropriate temperature for storing/transportation is freezing temperature.
• Stability:
After separation the plasma from cells, stability of the sample is defined in these conditions:
- In environment: unacceptable
- Second solidification (freezing): several hours to several days
- Freezing to -20 degrees centigrade: several weeks
- Solidification to -70 degrees centigrade: several months
11- Blood Sample Preparation Conditions
Vitamin C
• Exposure to sunlight, centrifuge and transporting plasma must be avoided and the blood sample must be freezed one hour after collection.
• Storage/transportation temperature: freezing temperature.
Vitamin A
Patient preparation: the patient must fast for 12 hours before the sampling and have to not consume any alcohol for 24 hours before the sampling.
Vitamin B6
Patient preparation: sampling must be done after one night of fasting.
12- Vitamin Assessment
Laboratory assessments:
• Concentration assessment:
- How much of the vitamin is present in the blood?
• Function assessment:
- Is the vitamin functions appropriate?
• Excretion assessment:
- Is there an extra amount of the vitamin?
• Indirect assessment:
- Whether the vitamin effects or its deficiency influences are present or not?
13- The challenges of the laboratory assessment of vitamins:
- Sensitivity to light (photosensitive chemicals) and temperature
- Problems in collection, transportation and storage
- Presence of vitamins in low quantities (pico molar/nano molar)
- High volume of sample is needed
- In some samples there is a high quantity of vitamins (in people who are ill or take supplements). Therefore, wide measuring range is needed for assessment of these types of vitamins. Also, samples must be diluted and the assessment must be repeated.
14- Laboratory assessment methods:
- Quantitative assessments
- Measuring each of the vitamins/vitamers
- Preparing the sample through protein elimination, extraction and derivation
- Separation with chromatography
- High Performance Liquid Chromatography (HPLC)
- Spectrometry/UV
- Fluorometry
- Electrochemistry
- Mass spectrometry
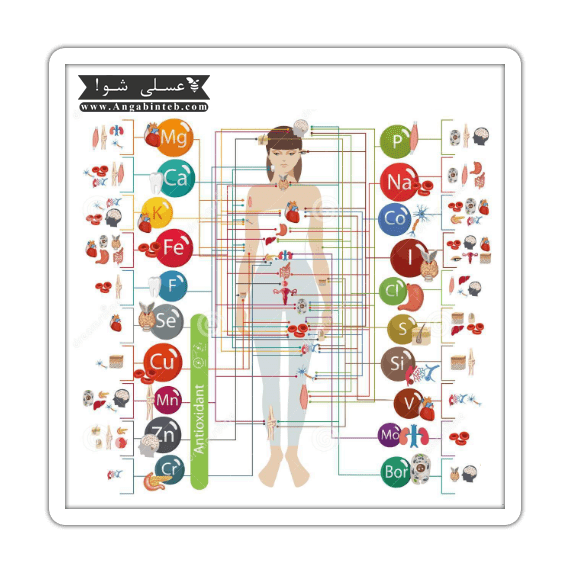
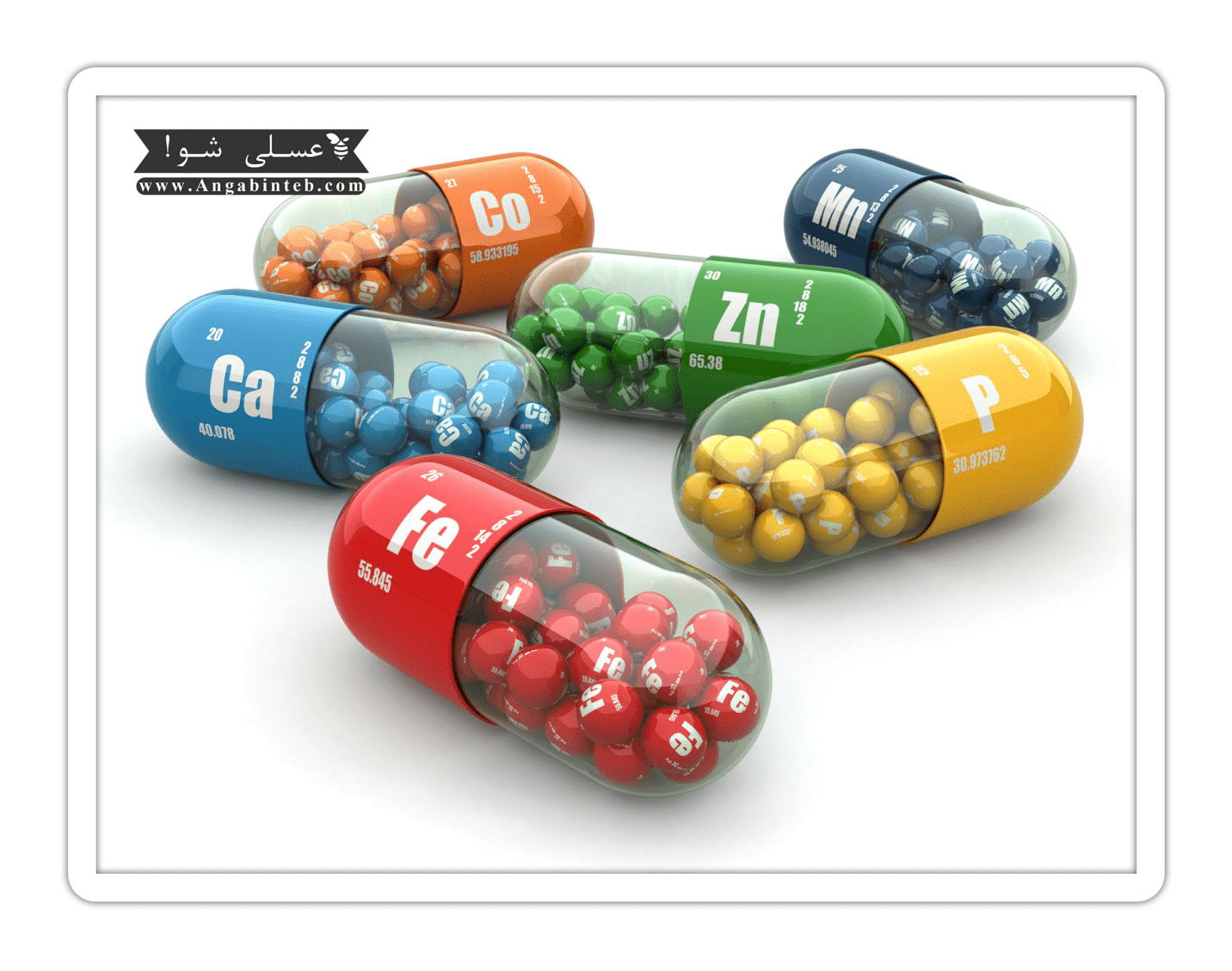
Part 2: Assessment of Minerals (minor elements)
1- Minerals definition:
Minerals are chemically minor elements with mean concentration less than 100 part per million (ppm) in atom counting or less than 100 microgram per gram.
In biochemistry, minerals are essential minor elements in diet that are necessary for body growth and proper functioning of organs in small quantities.
Minor elements are very important for cellular functions in:
• Biological levels
• Biochemical levels
• Molecular levels
• As a cofactor for many enzymes
• As a core for stabilizing the structure of enzymes and proteins
The human knowledge about the role of minerals in human body is less than 100 years.
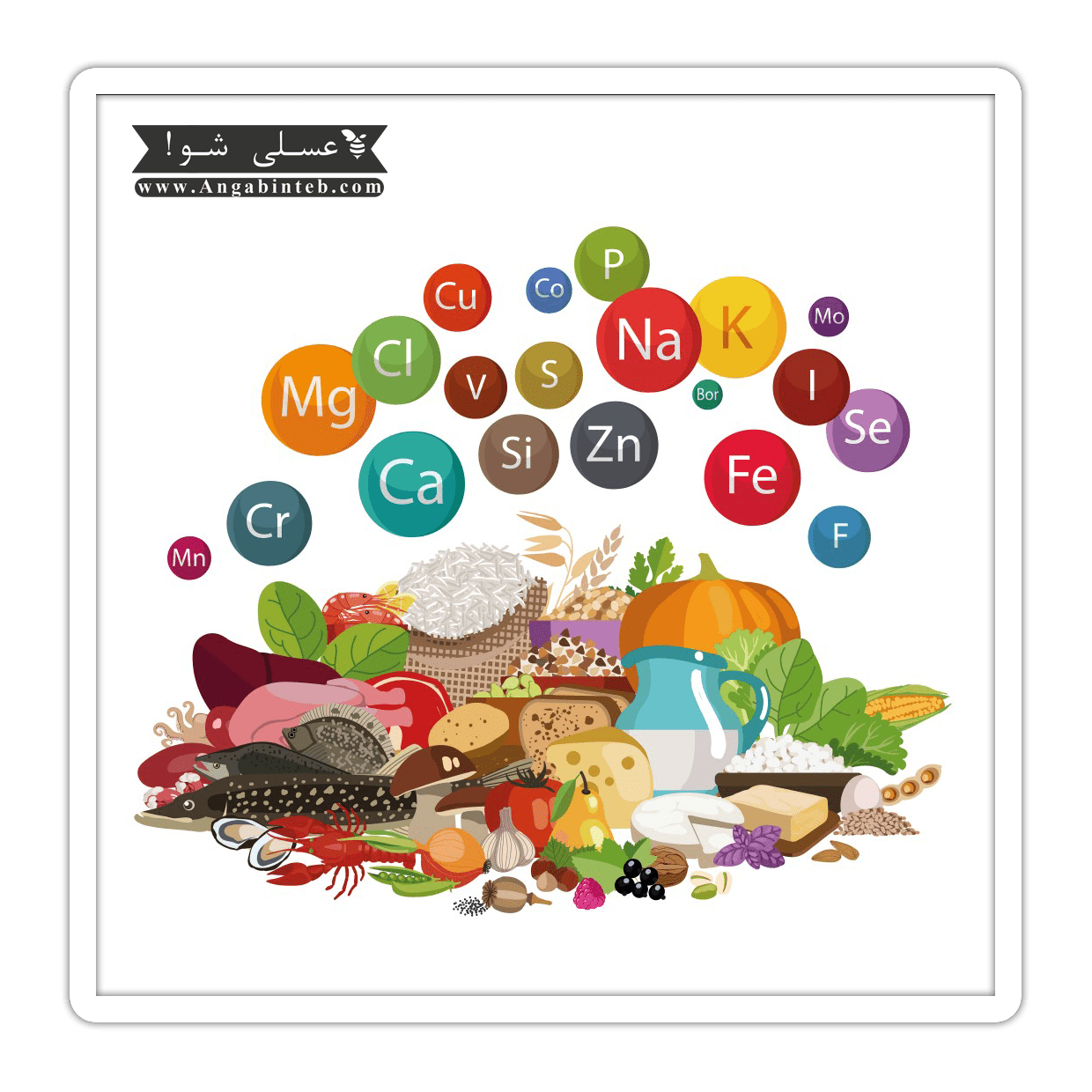
2- Necessity of minerals assessment:
1.88% of human body mass is made up of 4 main electrolytes sodium, magnesium, potassium and calcium.
The other elements constitute 0.02% or 8.6 gram of the average adult human weight. Although these elements only make up the 0.02% of the whole body weight, they have important roles in the body (enzyme activation centers or biological active substances). Accumulation or deficiency of minor elements might lead to changes in body function and disease, for this reason, assessment of minerals can be helpful in prevention or treatment of many diseases.
Deficiency or toxicity symptoms of several rare elements in the body are as the followings:
Mild zinc deficiency:
• Growth rate reduction
• Disorders in body ability to fight with infection
Severe zinc deficiency:
• Growth retardation
• Delayed puberty
• Delay in skeletal maturation
• Spreading of mouth and teeth dermatitis
• Diarrhea
• Alopecia
• Appetite suppression
• Behavioral changes
• Increase in sensitivity to infections (immunosupression)
Zinc toxicity:
• Nausea
• Vomiting
• Diarrhea
• Fever
• Malaise
Iron deficiency:
• Fatigue
• Weakness
• Headache
• Irritability
• Exercise intolerance
• Dyspnea
• Dizziness
• Chest pain
• Pica: The desire to eat nonfood items, which might be seen in many clinical cases and is not exclusively related to iron deficiency.
• Pagophagia: The compulsive consumption of ice or iced drinks; which is exclusively one of the iron deficiency symptoms.
• Beeturia: Redness of the urine after eating beet, which is not exclusively related to iron deficiency.
• Restless leg syndrome
Iron toxicity:
• Cardiomyopathy
• Hepatic cirrhosis
• Diabetes
• Arthritis
Copper deficiency:
• Cardiovascular diseases
• Bone disorders
• Neurologic and immunologic disorders in childhood and after that
• Prolonged mild copper deficiency in adults is related to changes in cholesterol metabolism
• Anemia
• Abnormal bone formation
• Osteoporosis
Copper toxicity:
• Effects of toxicity on gastrointestinal system: abdominal cramps, nausea, diarrhea, vomiting after consumption of beverage or water that contains a lot of copper
• Liver damage: it is exclusively seen in patients with Wilson's disease and children with hepatic cirrhosis
Manganese deficiency:
• Failure to thrive
• Reproductive disorders
• Glucose intolerance and changes in the metabolism of carbohydrates and lipids
• Decreased plasma manganese in women with osteoporosis is also reported.
Manganese toxicity:
• Persistent inhalation of high quantities of manganese is occurred in the air of mines
• Severe mental disorders (such as Parkinson's disease)
• Irritability
• Violence
• Hallucination
Iodine deficiency
• Infant death
• Low birth weight of infants
• Mental retardation in infants
• Decrease in IQ up to 15 scores in children
• Energy deficiency
• Goitre
• Hyperthyroidism
• Cretinism
3-Mineral assessment methods:
- Measurement of minerals concentration is conducted in body tissues, body fluids (intracellular and extracellular) and serum proteins.
- Assessment of enzyme activity of special elements in body fluids and tissues
- Studies on the balance of minor elements
- Biochemical and clinical responses to the prescription of the minor element
- Laboratory absorption of radioisotopes by tissues
4- Assessment of minor elements in tissues and body fluids (quantities assessment):
The sensitivity of modern analytic techniques including electrothermal atomization and atomic absorption (ETA-AAS) is sufficient for precise measurement of most minor elements in tissues and body fluids of healthy people. For this purpose the sample size must be acceptable (for example less than 5 milliliters of whole blood).
However the sensitivity of ETA-AAS is not enough for measuring the abnormal and low level of some minor elements such as serum cobalt. Chromium, molybdenum, vanadium and alternative biochemical indexes for identifying the deficiency of these elements are needed. Due to low levels of minor elements, high precision is needed for collection and processing of tissues and body fluids samples to prevent sample contamination.
The type of sample needed for measuring the quantity of different minor elements is different. For example, serum or plasma for copper, whole blood for lead, red blood cell or plasma for selenium and urine for arsenic. Choosing the best sample type among aforementioned samples, depends on the type of element; for example, albumin for zinc and alpha 2 macroglobulin for copper and nickel.
One alternative method for quantitative measurement of samples is laboratory analysis. Lead in bones and teeth is measured through fluorescence spectrometry of x-ray and cadmium in liver and kidney is measured through neutron activation analysis. These methods are used for the detection of these elements, if the patient has been exposed to high quantities of these elements.
5- Enzymatic assessment of minerals:
These assessments are not possible without the quantitative assessment of the minor elements concentration. In this method as well, the selected sample type is dependent on the type of element that is going to be measured. For example, alkaline phosphatase for zinc and` glutathione peroxidase of red blood cell for selenium. The collection and storage need careful control.
6- The balance of minor elements
This type of assessment is usually done in a 3 to 5 days period during which, the repetition of receiving any foods and beverages, and the excretion of any waste material is assessed through collection of the substances in urine and stool (identification through stool markers). For prevention of unwanted contamination with scarce elements while collection and storing the sample, intense caution is needed. In addition, especial equipments like titanium mixers and titanium homogenizer are necessary for elimination of contamination by elements like chrome during process and before analysis. These requirements usually limit the application of studies on balance of scarce minerals in specialized research laboratories.
7- Dynamic tests (kinetic):
Biochemical response to oral prescription of scarce minerals, similar to glucose tolerance test, might more easily provide information about intestinal absorption, compared to the balance of minor elements method. Recent development in mass spectrometry in plasma has provided the possibility of in vivo tests by using stable isotopes instead of radioactive. This precise tool is very expensive and is therefore limited to a couple of laboratories.
8- Absorption of radioisotopes by tissues in laboratory environment:
These tests are designed for identifying disorders of absorption or transportation of minor elements to biopsy samples and are usually conducted as confirmatory tests rather than research tests. For example, absorption of zinc-65 in biopsy samples of mucus membrane of intestine is considered as the confirmation of absorption disorder of zinc in Acrodermatitis enteropathica.